
Building a New Place for Mom & Dad
Building a New Place for Mom & Dad
The "silver tsunami" of baby boomers entering their senior years demands new solutions for housing and caregiving. A pioneer in assisted living shares lessons from her work and a promising vision for the future.
In 2002, the same year I founded the Jessie F. Richardson Foundation (JFRF), the National Institutes of Health published a report calling attention to the “2030 Problem,” the year in which the last Baby Boomer will turn 66 and the oldest Boomers will reach their eighties. The authors outlined the urgent need for communities to make significant changes in housing, health care, and human services if they intended to meet the needs of their aging citizens.
Now, more than fifteen years later and halfway to 2030, we still lack the solutions needed to avert a crisis in elder care. More ominously, we are short on innovative approaches. It’s not money we are going to need as much as an infusion of creative ideas and sustained attention.
Those beliefs energize our mission at JFRF: to empower communities, in resource constrained areas, to provide multi-generational support for underserved older adults. As an operating foundation, we are built on a core expertise in developing innovative housing solutions for seniors. We work by allying directly with local leaders in and out of government to foster and focus local resources toward strengthening and innovating local solutions.
What makes us confident this approach can serve the needs of an aging world?
When assisted living was far-fetched
I first learned how swiftly a simple idea can address systemic challenges in the 1980s. At the time, assisted living as we know it today did not exist. Old and disabled people were generally cared for at home until it was time to move to the nursing home. Nursing homes were organized like hospitals – no private space nor belongings, long hallways, and nursing stations under fluorescent lights. I know this setup intimately because my mother suffered a stroke at age 55 when I was in college and for the next 10 years she lived in a nursing home bed. Even as a young adult, it was easy for me to see that nursing homes were designed not for the comfort of patients but for the convenience of their caregivers.
In less than five minutes, Momma laid out the basic principles for the “revolutionary” model of assisted living we know today.
When I told my mother I was beginning a doctorate in Gerontology, she asked me a simple question: “Why don’t you do something for people like me?” From the mountains of east Tennessee, my mother had raised my siblings and me alone after my father died. She was a tough and independent woman.
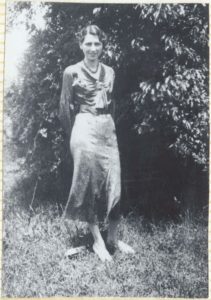
The author’s mother and namesake of the Jessie F. Richardson Foundation. Credit: JFRF
“Momma, what is it you want?” I asked.
She was clear: She wanted her independence back. She wanted her own place, her own kitchen, her cat, a place where she could smoke and be able to lock the door. In less than five minutes, Momma laid out the basic principles for the “revolutionary” model of assisted living we have come to know today.
Inspired by my mother’s vision, in 1979, I began to lobby providers and public officials to create a new kind of housing for the elderly in my home state of Oregon. With no takers, in 1981 my husband and a friend cobbled together funding to build the first 127-unit apartment building and fought for a special state waiver to license it. Three years later I finally got a waiver to do a demonstration project, using Medicaid funding. Not so shockingly, we proved that assisted living could provide less expensive, safer, and more dignified long-term care for the elderly. By 1988, new rules had been written, a statewide Medicaid waiver was in place, and I opened the first licensed assisted living residence in the United States.
It didn’t take long for people to realize that my Momma was just like a lot of Mommas. A wide range of private development funding followed, which enabled developers to go from single projects to national projects and economies of scale. Today, more than two million people live in thousands of assisted living centers in communities nationally.
The limiting factor hadn’t been cost, but vision; the stubborn barriers had been entrenched beliefs codified as policies.
Where will the aged live in rural America?
Today, one of the most stubborn misconceptions we encounter is the notion that Medicare and Medicaid are enough—maybe more than enough—to meet the long-term care needs of aging Americans. In reality, Medicare only covers brief stays for skilled nursing care and Medicaid has both financial and disability criteria that restricts its use, generally, to licensed long-term care settings. This leaves a gap between home and long-term care.
Americans want to age in place, in their own homes or in their communities. But what does that mean in a place like Oregon, where in many rural counties 30 to 40 percent of residents are 65 and older? “In place” could mean being hours from medical care, a clinic, or a pharmacy. The grocery store might be 60 miles away.
And who will provide care for these seniors as they age? Nationally, among the elderly who require assistance with daily activities, 65 percent rely exclusively on families and friends, and another 30 percent rely, at least in part, on informal care. In rural America, however, many members of the younger generation have left for education or jobs and probably aren’t coming back.
Forget about “aging with dignity.” The situation is more urgent.

Rackleff House (now Rackleff Place) in Canby, Oregon, developed by the author as the first licensed assisted living community in the nation. Credit: JFRF
Tapping underused assets
At JFRF, we work to address this national challenge through Asset Based Community Development (ABCD), an approach that seeks to amplify existing gifts and capacities of local “champions” and energize change and development from within. This means focusing on a community’s strengths versus solely its needs.
Every community in the country has unrealized community assets that range from human skills and knowledge to built structures and natural resources. School buildings are used less than half the time and rarely in the evenings. Buses sit in parking lots except for a few hours; the school cafeteria goes dark at 2 pm. Local fire fighters, paid or volunteer, are trained, trusted professionals who could lend their skills to deliver care to the chronically ill. The same is possible with retired teachers, nurses, and mechanics.
That’s why we focus on helping communities identify their priorities around aging and organize under-utilized resources in a systematic way. In almost every community, transportation, housing, and access to health services top the list of most critical needs.
A new solution: Housing with services
The most urgent need we see is for a new model of non-subsidized, suitable housing. In the past year, we have been hard at work on a solution that combines innovative building strategies, community/neighbor-based service delivery, and light health related services. We plan to pilot the effort in Oregon with hopes of expanding once we demonstrate success. Our vision is to create an affordable, sustainable model for senior living that is less reliant on or independent of subsidies. This model integrates new service approaches and existing resources, informal care systems with technology and embedded building features.
What does that look like? Imagine a system where a neighbor can exchange work or skill for a rent or service credit. Maybe Mrs. Jones can prepare meals for the elderly couple in apartment 4D in exchange for reduced rents. Structuring a sharing economy will strengthen mutual and intergenerational connections and create more interdependence. Already, technology for app-based home care-giving is being piloted by folks like Home and Care, who can provide inexpensive and accessible support—like medical advice, health reminders and more—to individuals living far from providers.

In rural communities, “aging in place” poses unique challenges. Credit: JFRF
Scaling the concept of housing with services is daunting but doable. Foremost is the need for new financing options. By demonstrating attractive returns through pro forma financial statements, we can uncover new mechanisms that allow financial institutions to offer loans and government entities to float bonds. And many rural communities—short on cash but rich in undeveloped land—might seek land trusts to help pay for new housing options.
We also need to support a different type of builder, developers for social good, who offer design and building services based on fixed fee, not as a percent of construction costs. Building plans and purchasing are easily scalable. In theory, we might consider developing delivery models similar to the days when Sears and Roebuck transported new houses on rail cars, or even produce housing with 3-D printer technology that exists today.
Our approach may seem overly optimistic. But to me, it doesn’t seem any more far-fetched than the creation of assisted living. Moreover, we are confident in the ABCD approach because we have seen it work on the ground. More than 15 years ago, our foundation began working to change elder care in Nicaragua, one of the poorest countries in our hemisphere. We partnered with local groups to create interest in the plight of the indigent elderly, and focused on growing community support of hogares, homes for poor, elderly Nicaraguans. Grassroots councils emerged to care for townspeople. We fostered intergenerational involvement in support of the old. Currently, we are working with U.S. and Nicaraguan university systems in the curriculum development and training of a new generation of professionals to serve the care needs of the aging population.
People are always surprised by how many assets they have in their community. Mostly those assets are simply other people who together possess much of the knowledge they need to solve their own problems. What they need help with is analyzing their experiences, assessing their knowledge, and translating that knowledge into action. When local communities organize around an issue they can accomplish remarkable things. And the wonderful thing about our work to support older adults is that our elders are our richest—and most neglected—resource. They’ll pay society back in spades.
Keren Brown Wilson, Ph.D., is founder and president of the Jessie F. Richardson Foundation (named in honor of her mother) in Clackamas, Oregon.
Project
Innovative Housing Solutions for Seniors


